Pancreatitis is a dangerous condition where the pancreas becomes inflamed. Fitness enthusiasts who have suffered acute pancreatitis are often left wondering whether it is safe to lift weights after pancreatitis. It is, but you may need to change your regime and take some precautions.
There are two types of pancreatitis: chronic pancreatitis and acute pancreatitis.
But before we look at the different types of pancreatitis, let’s first go back to biology class as we answer the question: what is the pancreas?
What Is The Pancreas?
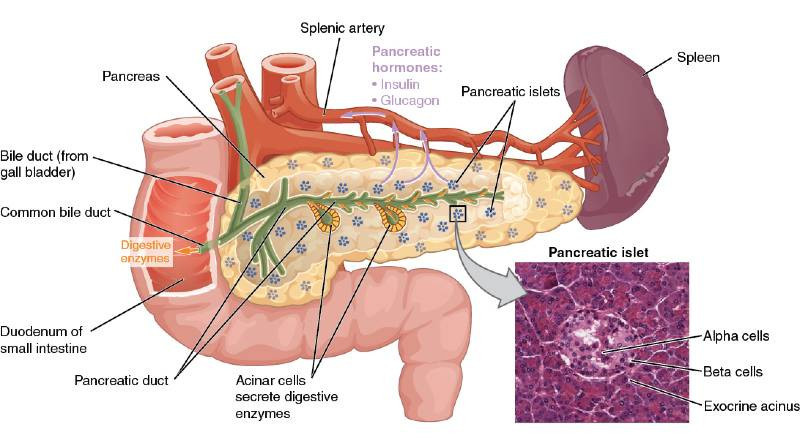
The pancreas is a gland which measures around 6 inches and is situated deep in the abdomen. It is surrounded by the stomach, small intestine, liver and gallbladder.
The pancreas has two functions: to aid with the digestion of fats, carbohydrates and protein by the release of pancreatic enzymes; but also to produce hormones that help regulate blood sugar.
So now that we know what the pancreas does, where it is situated and and why it’s a vitally important organ, let’s take a look at both chronic and acute pancreatitis.
Chronic Pancreatitis
Chronic pancreatitis is the long-term inflammation of the pancreas which causes debilitating abdominal pain that radiates through to the back.
The most common cause of chronic pancreatitis is long-term alcohol abuse, but other lifestyle factors can also play a part. Smoking, for instance, is thought to prolong chronic pancreatitis as it causes the gland to harden.
While there can be genetic factors that cause chronic pancreatitis, this is very rare. At the risk of generalising, it is reasonable to say that chronic pancreatitis tends to be caused by unhealthy lifestyle choices.
The focus of this article will be on acute pancreatitis answering the question can you lift weights with acute pancreatitis?
Acute Pancreatitis
As with chronic pancreatitis, pancreatitis is the inflammation of the pancreas but where the inflammation lasts a relatively short period of time.
Acute pancreatitis has been linked to gallstones and excessive alcohol consumption.
Many people who suffer from acute pancreatitis are going to make a full recovery within around a week. However, the condition is prone to complications such as necrosis, which can be fatal.
So acute pancreatitis is a serious condition that will definitely put a halt to your workout regime while you recover.
But before we look at some of the things you can do to accelerate your recovery from pancreatitis, I’m going to tell you from first-hand experience what pancreatitis feels like.
Fit And Healthy Before Pancreatitis
The year was 2013.
I had completed the P90X program a year earlier, in 2012, which had completely revolutionised my approach to exercise.
Prior to that I had been the stereotypical gym rat who would labour through sessions focused on individual body parts, lifting as heavy as possible in the 5 to 8 rep range.
Most of those sessions we spent changing plates, looking in the mirrors and catching up with my fellow gym rats!
P90X had brought an intensity and efficiency to my workouts that I couldn’t let go of.
But moreover, I had become interested in my overall health and fitness as opposed to building over-sized muscles.
This had led me on to take up running and in October of 2013 I completed a timed 10k coming in at just under 50 minutes, which considering I had never been able to run before, I was very pleased with.
The other thing that I had changed in 2013 was my diet. In the spring of that year, I succumbed to the hype and decided to go plant-based.
I was fastidious in my diet research and made sure that I was consuming sufficient protein, vitamins and minerals every day and did my utmost to eat only whole foods, rather than fill up on processed vegan junk food.
test
It might be your pancreas
Before we dive deeper into the warning signs of pancreatitis, let’s pause for a moment.
If you’re looking to expand your understanding of this condition, ‘It Might Be Your Pancreas: Pancreatitis Awareness and Natural Digestive Recovery‘ by Diane Greco Allen, is a treasure trove of insights.
This audiobook takes you beyond the basics, illuminating the root causes and offering natural recovery methods.
Best of all? You can listen to and keep this invaluable guide for free! It’s an opportunity you shouldn’t pass up – enhancing your knowledge at no cost is truly a no-brainer.
Let’s now explore the warning signs I was experiencing that, had I listened to them, may have averted the most painful illness of my entire life to date.
5 Early Warning Signs Of Pancreatitis
There were a number of changes that occurred during the run up to my hospitalisation with acute pancreatitis.
I’ll go through each of them with you now, starting with the earliest to those immediately before the attack.
Before I do, however, I want to say that these were the early warning signs that affected me. Don’t wait to see a doctor if you suspect you may be suffering from pancreatitis just because you’ve not experienced one of these warning signs.
1. Weight Loss
Whether it was the new running regime, the change to a plant based diet or combination of the two, by September of 2013 I was looking increasingly gaunt.
At the beginning of 2013, I weighed around 73kg and this had dropped to around 67kg by September.
Looking back at photos from that time, I looked unnaturally thin and this didn’t go unnoticed by colleagues and friends who counselled me to start eating meat again.
It was painfully obvious to them that I wasn’t thriving and they were blaming my dietary choices.
2.Decreased Tolerance To Alcohol
I recall that around late September, early October of 2013 I was out with some lawyers I referred work to for some after-work drinks.
I wasn’t a big drinker at this stage. Having partied hard in my 20s and now with a young family as my priority, the demon-drink had lost its appeal.
On this particular evening however, I remember feeling drunk before I had reached the end of my first pint.
In fact, the effects of the alcohol were so disturbingly powerful, that after that first pint, I made my excuses and made my way home, the world swimming in and out of focus as I did so.
3. Steatorrhea (Oily Or Greasy Stools)
There’s not too much talk about this one in articles about acute pancreatitis perhaps that’s because it’s gross.
Let’s face it nobody wants to talk poop!
But as I look back this is probably the most clear warning my body gave me that my pancreas was not in a good state.
I thought that my foamy green stools were simply the result of eating lots (and I mean tons) of green veg.
But the giveaway was the oily film when I looked down in the toilet bowl.
4. Nausea
I’ve always hated being sick, but in reality, it’s nausea that is the worst part of being sick and usually, once you’ve vomited, you begin to feel better.
With pancreatitis though, you are faced with persistent nausea that just won’t go away.
You cannot eat and have no appetite whatsoever.
The nausea tends to increase and intensify over time too – often spanning days.
5. Pain
I’ll go on to detail the pain I experienced in the next section, as it wasn’t typical of how pancreatitis is usually felt.
In most cases of acute pancreatitis, sufferers will experience pain in the gut – it may start as indigestion, but then get more severe and radiate into the back.
What Does Pancreatitis Feel Like?
So you understand my background of exercise and dietary changes leading up to my bout of acute pancreatitis and you know the warning signs that my body had been giving me.
We will now go to the night of the office Christmas party in December 2013 where I’d finished my fifth pint and was ordering a whisky as a nightcap.
I was very drunk and amusingly flatulent!
Yes, that’s right! Over the previous month I’d developed a lot of flatulence which once again, I’d attributed to the plant based diet I was following.
I managed to get myself home on the Metro and stumbled through the front door where my wife got me a cup of tea and sent me to bed!
I fell asleep that night, knowing that I was in for a hangover from hell the next morning.
So imagine my surprise when I woke up relatively early the next day, feeling very fresh and not at all hungover!
Well, that wasn’t going to last.
By late afternoon, I’d begun to feel nauseous and I didn’t eat anything that evening. I put this down to a delayed hangover and sipped water to try and quell the sickness.
An early night ensued and I fully expected to wake the next morning fully recovered.
When I awoke however, I found that the nausea had increased and I was feeling truly awful.
The nausea increased during the day, to the extent that I attempted to be sick, but couldn’t.
I had also begun to experience a deep, dull throbbing in my kidneys and knew instinctively that something was very wrong inside me.
I trotted off to the medical centre to get looked over, and was sent home with antibiotics for a suspected kidney infection. Not good.
The next day was Christmas day and by this time, I was extremely poorly.
The nausea was causing me to wretch but nothing would come out.
The pain in my kidney area was so severe that the ONLY position I could get comfortable was to be flopped – chest down – over a beanbag.
I couldn’t sleep because of the pain and the nausea, and if I did drop off, I would be awoken by a pain unlike anything I had ever felt.
This pain felt as if somebody had taken a drill to my kidneys.
It caused me to wake, screaming in agony.
On Boxing Day, I went to the emergency room where they took blood from me. When the results showed that my kidneys were on the verge of failing, they admitted me to a ward.
Over the next four days, my kidney function bounced back and I was discharged – albeit without a diagnosis.
The trauma of what I had just encountered deeply affected me.
I was petrified that this could happen again.
It took 3 months for me to receive a diagnosis, thanks to the wonderful nephrologist I was under, who reviewed the original bloods that had been taken at the emergency room and identified the tell-tale signature of elevated amylase levels that nobody else had picked up on.
I was back out running within a month. But was that the right course of action? Well, keep reading and you’ll find out.
How To Recover From Acute Pancreatitis (The 3 F’s)
In this section we will look at my “3 F’s” of recovery. I warn you that there will be some religious and spiritual content in the first of these F’s – Faith – but PLEASE don’t skip.
It might be your pancreas
In the journey to recovery, knowledge is your best ally. That’s why ‘It Might Be Your Pancreas: Pancreatitis Awareness and Natural Digestive Recovery’ by Diane Greco Allen is a must-have.
This audiobook sheds light on holistic nutrition and medicine’s power to heal, shared through the author’s personal and professional experiences.
And the best part? You can access this wealth of information for free, keeping it forever. Enhance your recovery process by embracing this no-cost opportunity to learn from a seasoned expert.
1. Faith
At the point in my life when I suffered this attack of acute pancreatitis, I was 34 years old and had been an atheist for most of my life.
I came out of hospital overwhelmed with fear that what had happened could happen again at any point.
That fear only increased when I received the diagnosis, 3 months later, and I began researching acute pancreatitis.
And for the next 6 years, fear and an awareness of my own mortality overshadowed my whole life.
The fear caused anxiety, which led to other stress-related conditions, such as gastritis. And given the overlap of some of the symptoms of gastritis, you can imagine the panic that this would cause internally.
In 2019, it all got too much and one day in April of that year, I found myself listening to Derek Prince preach on the Bible. After hearing what he had to say, I called out to God and can honestly say that He has answered.
My faith in Jesus Christ, who is my redeemer and my healer, has been the key to my full recovery and moreover, He has eradicated the oppressive fear and anxiety that stemmed from the horrific episode of acute pancreatitis.
He’s also opened many more doors for me that I “may have life and life more abundantly”, so please don’t discount what I’ve written here.
I would say that faith in Jesus Christ has been the most important factor in my recovery.
2. Food
Once I had received the diagnosis of acute pancreatitis, I was able to research the lifestyle changes I needed to implement to avoid a recurrence and help my pancreas to heal.
One of the first things I committed to doing was to begin eating meat again. In fact, I vowed never again to impose any kind of exclusion diet on myself.
I accepted that humans are, by design, adaptable and intelligent omnivores capable of applying cooking and preparation processes to foods they would otherwise by inedible.
I also vowed I would never again be a glutton. When I look back on the way I used to eat when I was a wannabe bodybuilder, I cringe with shame.
So a healthy relationship with food is a definite prerequisite to healing from acute pancreatitis.
But you also need to give the pancreas time to heal and so you want to lighten the load of work that it has to do.
I still follow these general principles today:
- Start the day with 1 tbsp of live Apple Cider Vinegar in 500ml water, 30 mins before eating;
- Eat lean meat (unprocessed chicken and beef boat digest well);
- Eat a small to moderate amount of salmon & sardines and larger portions of white fish at least 3 times per week;
- Avoid fried and deep fried foods;
- Eat a good amount of steamed green vegetables every day;
- Try and consume at least one portion of legumes per day (canned chickpeas or green lentils in a salad work well);
- Eat a portion of blueberries, or other berries every day;
- Start using turmeric, ginger, cumin and other spices which have anti-inflammatory and healing properties. They are potent, so there’s no need to overdo it.
The ACV and the legumes will help to naturally lower your blood sugar levels – reducing the load on your pancreas.
The other measures are simply foods which I have found to be easy to digest and which deliver a serious amount of nutrition.
In fact, I can tell you that I now suffer less indigestion than I ever have, so please, if you’re recovering from acute pancreatitis, take comfort from my example.
I would also recommend sourcing a good quality multi-spectrum digestive enzyme for the first 6 to 12 months after pancreatitis as these can help, particularly when you eat fattier meals.
3. Fitness
It pays to look after the body and exercise is one of the best ways we can do that.
The scientific research into the benefits of exercise is vast and there are plenty of specific benefits for pancreatitis sufferers that compel me to recommend exercise as part of your recovery from pancreatitis.
Before we look into how you should exercise after pancreatitis, I just want to mention a couple of scientifically proven benefits that should convince anybody who has suffered from acute pancreatitis, not to throw in the towel on their exercise program.
- Exercise has been shown to combat Type 2 diabetes and provide health benefits to those with Type 1 diabetes.
- Regular exercise improves insulin sensitivity.
- Exercise reduces the risk of cancers, including pancreatic cancer.
- Exercise may reduce gallbladder risk by around 30%
Exercising With Pancreatitis
So let’s bring all of this together and answer the question most of you came here to know the answer to: is it safe to lift weights after pancreatitis?
We’re going to look beyond that question though, and consider both cardio and strength training, as I have found a very insightful article that I’m going to share with you – and it certainly ties in with my own experience.
How long Should I Wait Before Exercising After Pancreatitis
I was back pounding the pavements just four weeks after my hospitalisation with acute pancreatitis.
However, I wouldn’t recommend this as I was significantly weakened by the acute pancreatitis. Intense exercise seemed to take a heavy toll on me in those early days.
This would take the form of exhaustion and discomfort in my back – especially when sitting.
I would recommend instead that as soon as you are out of hospital and feel up to it, commit to a walking program.
Start small and build up over time. You could use your first hour upon waking in the morning as a time to go on your daily walk and over time, perhaps even add in an evening walk too.
Walking can be a great time to catch up with podcasts, or in my case, a great time to pray! But it can also be a great opportunity to catch up with friends too, so why not make it part of your social life.
You’d be amazed at how quickly 5k passes by when you’re catching up with a friend.
Lifting Weights After Pancreatitis
Lifting weights after pancreatitis is generally safe, however you may wish to limit exercises where there is an increased risk of raising internal pressure.
These are exercises such as squats, deadlifts and overhead presses.
Of course you don’t necessarily need to completely exclude these exercises, but it may be sensible to lighten the load and only work them in the +20 rep range.
All other lifts should be safe – again with the caveat that lower weights and higher reps is preferable during your recovery.
In my own case, I waited 12 months before trying to add any weights to my lifts. I found it satisfying enough to simply get some tone back and acquire just a little muscle while I was recovering.
I would highly recommend investing in some adjustable dumbbells as there is an astonishing array of exercises you can compete with them and you will be limited in terms of the weight you can lift when compared to barbell training.
If your budget extends to it, you may want to consider investing in a functional trainer, given that they are so convenient, versatile and allow for full body workouts that are completely safe and effective.
Check out my recent article on 5 great cable machines that are suitable for a small home gym.
🏋️♀️ Lift Heavy, Live Well – The Shirt That Fuels Your Workout!
“If I can push past migraines, pancreatitis, and more to stay fit, so can you. Wear your motivation!”
👇 Click to Buy Your ‘Lift Heavy, Live Well’ Tee NOW! 👇
🔥 Limited Edition! 🔥
This isn’t just a t-shirt; it’s a badge of honor. Perfect for workouts, it’s designed to:
- Keep you inspired 💡
- Make you part of a like-minded community 🤝
- Remind you of your strength and resilience 💪
Limited stock! Click below to join our community of warriors!

Cardio After Pancreatitis
We’ve already explored the benefits of walking – and this is my number one recommendation for cardio when first recovering from acute pancreatitis.
Building up to 1 – 2 hours of walking per day, split into as many sessions as you want, would be a good goal to work up to.
However, any other low-impact cardio would also be advisable: such as cycling, stationary bike or elliptical trainer.
So what about jogging?
After all, I was back jogging within a month of acute pancreatitis. Was that a mistake?
In hindsight, I believe it was.
If you reconsider my exercise regime before pancreatitis, I had switched from a predominantly weight lifting regime to a predominantly running regime.
I appreciate that there were likely other significant factors: most notably the consumption of alcohol the night before my symptoms began, but also the switch from an omnivorous diet to plant-based, but I am convinced that running played a significant part in my bout of acute pancreatitis.
This conviction only increased when I read this article written by a gastroenterologist who saw the same guy – an avid runner – who repeatedly presented with acute pancreatitis.
I can sympathise with the runner: I can well understand why he was so reluctant to accept that it was the running causing his pancreatitis, but when I look at my own pattern and the discomfort I’ve experienced since, whenever I embark on a running program, I am inclined to believe that running simply may not suit some of us.
Lifting Weights After Acute Pancreatitis
We’ve taken a deep dive through the condition of acute pancreatitis and looked at the different lifestyle factors that can trigger an episode.
I’ve also shared with you the early warning signs that affected me before I was hospitalised with pancreatitis. It is my hope that these will be of use to you and your loved ones.
We’ve also looked at what you can do to expedite your healing from acute pancreatitis and we can conclude that not only can you lift weights after acute pancreatitis, but you should.
OK, so you may not be going for any personal bests in your lifts for a while, but keeping the blood flowing to your muscles and keeping your strength can only be a good thing.
Just make sure that you’re not unduly increasing your internal pressure and make sure that you review your workout plans (and this article) with your healthcare professional before embarking on your post-pancreatitis workout regime.

I am currently recovering from acute pancreatitis where in additions to other symptoms, resulted in a significant weight loss which was mostly muscle mass. I am considering going back to my workouts and found this article and your experience very similar to mine. Thank you for the pointers. This was very helpful.
Tom
Hey Tom,
First off, I want to say it’s great to hear from you and I’m really glad you found the article helpful. I can totally relate to your situation as I’ve been there myself. Recovering from acute pancreatitis and dealing with significant muscle loss is no easy feat and I want to commend you for your bravery and resilience. Remember, it’s okay to take it slow and steady.
In the early days of my recovery, I had to adjust my diet significantly. It was all about steamed veg and lean meats. I know it might not sound like the most exciting menu but trust me, it was what my body needed at that time to heal and recover.
Fast forward to today, I’ve been able to reintroduce a plethora of tasty, muscle-building foods into my diet. I’ve been experimenting with the ketogenic diet recently and I have to say, it has been a game-changer for me. I love the variety it brings and how it aligns perfectly with my fitness goals – but I couldn’t have contemplated this at the time of my pancreatitis attack and subsequent recovery.
Remember, everyone’s body and journey is unique. What worked for me might not work exactly the same for you and that’s okay. The most important thing is to listen to your body and adjust accordingly. You’re already doing a great job by considering going back to your workouts. That’s a step in the right direction, just don’t try to do too much too soon. You’ve got many years ahead of you to recoup the muscle you’ve lost and I’m sure, in time, you’ll be packing on more besides.
Yes, be assured that it’s more than possible to regain all the lost muscle mass and even surpass your previous fitness levels. It’s a journey, not a race. Believe in the process, keep moving forward, and the results will come.
Stay strong, Tom. Feel free to reach out if you need any more advice or just want to chat about your progress. Remember, we’re in this together.
Take care, Matt
To me, the worst part of recovery with this condition is convincing others that I am not well.
When I go out for something, and when someone asks me to help them with something heavy, I have to say no and walk away.
I can’t walk away fast enough, and it just adds to the stress. I know how a conversation with someone who doesn’t know about the condition would pan out.
Family is just as bad as strangers in that respect.
“You look well enough,” was something that made me resent the circumstances.
I’d say around 90% of the contacts in my phone are blocked.
Hi John,
I truly understand what you’re going through. During my recovery, I too faced immense challenges, like deep back pain that made even driving my relatively short commute a struggle. I even had to give up my beloved Mazda MX5 (Miata) for a more mundane, comfortable car and often had to stop and rest due to the pain. Like you, I felt misunderstood by colleagues and even my family at times.
Nobody understood the pain, the fatigue or the fear that another bout could be just around the corner.
But I want to reassure you that there is light at the end of this tunnel. It might be hard to see now, amidst the physical pain and the misunderstanding of those around you, but things can and do get better.
I’ve been where you are, feeling isolated and frustrated, but now I’m enjoying life fully again – exercising, eating well, and embracing each day.
Your journey might be tough now, but hold onto hope. Keep prioritizing your health and well-being, and remember that it’s okay to take the time you need for yourself. Better days are ahead, and you will find your path to a full, enjoyable life just as I have.
Stay strong, and know that my family and I will be praying for you.
To your health,
Matt
I have been back to the gym for over a year and am having a really hard time trying to build any muscle. My shoulders still look small and weak and so does my chest. I am stronger but you would never know I had set foot in a gym. Very frustrating. I should be happy that I’m feeling so good however.
J C
Hi J C (wow, I love those initials!!),
Thank you for stopping by and sharing your experience.
I’m not sure how long it’s been since you suffered from pancreatitis, but remember, time really is a healer. Take it easy on yourself and listen to your body as you start to increase your protein intake.
I’ve found that I do best on a low-carb, high-protein diet that’s completely free from processed foods, refined sugars, and sugar alternatives. It turns out, such a diet is also excellent for building muscle.
Here’s another hack for you to try: timed workouts. Grab an interval timer and set it for 8 rounds of 35 seconds, with 40 seconds of rest in between. Start with dumbbell shoulder presses for your first 8 sets, then move on to dumbbell flies, and finish with bent-over rear dumbbell flies. Aim for 8-12 reps per round. That’s about 30 minutes of pure shoulder pump.
This approach has been transformational for my own delts, and I hope, coupled with a low-carb diet, you’ll see outstanding results too.
One last thing: I’m just about to update this article with an audiobook I’ve been listening to on the topic of pancreas health. I think you’ll find it incredibly insightful, and the best part? It’s yours to keep for free!
To your health (and gains)!
Matt